Overview
The shoulder joint is a ball and socket joint. Shoulder instability is diagnosed when the ball slips or completely dislocates from the socket.
There are two main types of shoulder instability, both of which can present in a range of ways. One is traumatic instability, which can happen if your shoulder is hit, perhaps in a fall or in an accident. The other is atraumatic instability. This can occur in some people simply because they have "loose joints", or it can develop over time as the result of specific repetitive movements.
If your shoulder joint slips, it is known as subluxation. You may feel the ball slipping, catching or coming out of its joint. This can be associated with pain and a sense of a "dead arm". It may also make you feel apprehensive about moving your arm in certain positions.
If the ball comes completely out of the socket of your shoulder joint, it is called a dislocation. With a dislocation, you may not be able to put it back in to the joint yourself. A dislocation is also more likely to damage the structure of the shoulder.
Your instability may get worse over time. It is possible to get both dislocation and subluxations in the same shoulder. For example, after having dislocated your shoulder in a fall and had it relocated in hospital, you may find the joint slipping when you try a particular activity, such as throwing a ball or swimming.
Why does it happen?
Traumatic instability
Traumatic instability happens when your shoulder joint collides with a hard object or your arm is forced into a particular position. For example, if you hit it on the ground in a fall, if something bangs into your shoulder in a car accident, or if someone collides with you in a rugby tackle. The ball socket is normally pushed forwards and downwards, usually when your arm is out to the side and twisted backwards. Traumatic dislocations can result in damage to the labrum and recurrent instability.
In a very few instances the ball may be forced out backwards (posterior dislocation). This tends to occur if your arm is in front and across your body on impact. Unfortunately having had this injury once, it tends to recur. Research also shows that the younger you are when you have the first dislocation, the more likely it is to recur.
Atraumatic instability
For some people the shoulder is not involved in a specific accident or event, but the joint gradually feels unstable. This may develop with specific, repetitive movements of the arm (such as throwing balls or swimming). Sometimes people have "loose joints" and these can become a problem and start dislocating or slipping during everyday activities.
The ball may slide forwards (anterior), backwards (posterior) or downwards (inferior). Sometimes it may slide in more than one direction and occur in both shoulders.
A few people can make the muscles pull the ball out of the socket, without moving the arm at all. This is known as "voluntary" dislocation. Often it starts as a party trick but can cause the joint to slip out involuntarily. Do not do this movement! It trains the muscles incorrectly and reminds your brain of an incorrect movement. You will probably always have the ability to do this; however, our advice is not to make use of that ability.
Sometimes it is not clear-cut as to whether you have a purely traumatic or an atraumatic instability problem. The two situations can overlap to some extent.
How common is it?
Because the shoulder joint is the most mobile joint in the body it is potentially unstable. It is therefore the most common joint to dislocate in the body.
Symptoms
You may feel a popping, locking or grinding sensation, often with some pain. A symptom of chronic instability often includes the feeling that your shoulder may come out of its joint when your arm is in a certain position.
You may have had a history of a traumatic dislocation and the current episodes of injury to dislocate the shoulder. Depending on the damage done the shoulder may feel like it is coming out of the joint or slipping more frequently or easier with time.
Investigating the problem
Physical examination
Mr. Cole will talk to you about your shoulder symptoms and your shoulder’s history. He will examine your shoulder and assess your range of movement. He will put you arm in certain positions and will perform the clinical instability tests. This normally provides sufficient evidence for a diagnosis to be made. However, he may wish to see an x-ray or an MRI Arthrogram scan of the damaged shoulder.
X-ray
An x-ray can provide an excellent ‘picture’ of bones and joints and will clearly show any dislocation or subluxation. It may show previous damage to the bone suggestive of previous dislocations or subluxations such as a Hill Sachs lesion (a ‘dent’ in the head of the humerus)
MRI Arthrogram
Especially in cases of traumatic instability, there may be some damage to the shoulder’s rim of cartilage, ligaments, tendons and muscles. An MRI can highlight any damaged areas.
MRI stands for Magnetic Resonance Imaging. It uses a powerful magnet to obtain three dimensional pictures of body structures. In cases of instability the accuracy of the investigation is significantly improved with an injection of gadolinium into the joint (Arthrogram).
Treatment options
The treatment you are offered is dictated by the kind of shoulder instability you have. If you have just dislocated your shoulder for the first time, you may be advised to rest it and keep it as immobile as possible in a sling to allow your damaged tissues to heal and pain to subside. After this you will be given a course of physiotherapy to strengthen the shoulder, regain movement and reduce the feelings of instability.
Treatment for traumatic instability
If your joint is stiff or the muscles weak when tested, you may be sent for a trial of physiotherapy. However, if the movement is good and muscles are working well but the joint is dislocating or slipping regularly and stopping you doing what you want to do, Mr. Cole may offer you an operation. This is called an anterior stabilisation operation. You will be given further details on this operation if this option is given to you. Dislocations and subluxations caused by trauma often give ongoing problems and 50% of people will need an operation to stabilise the joint. The operation has a high success rate.
Treatment for traumatic instability
You may be recommended for a course of physiotherapy. Surgery is not recommended unless an extended, appropriate course of physiotherapy has been given and has been unsuccessful. Surgery is not always helpful; in fact it can make some people in this category worse, so it is important that you work hard at the physiotherapy. It will only work if you do your exercises assiduously.
In the unlikely case that you are offered surgery, Mr. Cole will discuss the different options with you. The joint can be stabilised with an ‘open’ stabilisation operation – where the joint is opened and the capsule tightened or as a keyhole (arthroscopic) procedure. You are less likely to be offered surgery if you can voluntarily dislocate your shoulder as the research tends to show poor results in this group of patients.
Physiotherapy
Your physiotherapy will have several broad aims. These include retraining your body to move in a particular way, strengthening your muscles, retraining your body’s sense of position and enabling you to return to sport and activity.
Retrain movement
This is probably the most important aspect of your treatment. The emphasis is on getting the optimal movement of the shoulder blade (socket) and arm bone (ball). Some people may have developed unusual movement patterns which need to be corrected.
Strengthen muscles
Initially the aim is to regain control of your muscles around the shoulder blade and the deep muscles around the ball and socket joint. Muscles that are weak or get tired easily need to be strengthened.
Retrain ‘position sense’
The unstable shoulder can have a reduction in the ability to know where your arm or shoulder is in space. Certain types of exercises may help retrain this.
Return to sport or activity
Once the control, muscle endurance and strength have improved you will be slowly guided back into positions or activities where the shoulder was feeling unstable. In addition if you have pain, or stiffness, or both, there are treatments that may help you.
How long do I need to do the physiotherapy exercises?
You need to do your exercises at least three times a week to give them any chance of working. Ideally, try and get into the habit of doing them every day, then it does not matter so much if you miss an occasional day.
In addition, you need to continue with the exercises over a minimum of 12 weeks. If your muscles are weak it will take this length of time for them to respond to the exercise programme.
Your response to physiotherapy will take some time. You may not see any changes for six weeks, for example, even though you are doing your exercises regularly. If your condition does not respond to physiotherapy, Mr. Cole may discuss the surgery options with you.
In addition, you may also find that if you stop doing the exercises the problem has a tendency to return. Therefore you may find that you will need to continue with some form of exercise forever.
Surgery
Arthroscopic stabilisation and open stabilisation
The operation
The first time you dislocate your shoulder, especially if the dislocation happened because of a traumatic event such as a fall onto an outstretched hand, your shoulder will normally be put back into position in A&E. Sometimes, a qualified medic may be able to put your shoulder back at the point of the accident. This may be on the rugby field, for example. You will normally be given painkillers or sedatives during this procedure.
When the first dislocation or subluxation happens (subluxation is where the shoulder only partly comes out of its joint), ligaments are often damaged at the front of the shoulder. In as many as 70% of people who have suffered from a dislocation or subluxation, this can lead to persistent shoulder instability. If you experience repeated dislocations or subluxations, you may need stablisation surgery. The surgery will repair or tighten these ligaments and any damaged muscles or cartilage.
Mr. Cole will discuss the best type of operation for your shoulder. Different types of surgery suit different injuries. Arthroscopic stablisation uses keyhole surgery techniques with a miniature camera. Open surgery is a more traditional form of surgery.
About arthroscopic stabilisation
The precise damage inside your unstable shoulder can vary enormously, from a torn capsule to labral detachments and bony damage to the glenoid. Arthroscopic surgery aims to repair anatomically the areas that are damaged. Sutures and anchors may be used to reattach and tighten torn ligaments and cartilage (labrum) around the socket part (glenoid) of your shoulder's ball and socket joint (glenohumeral). This procedure is most often used with people who have ongoing instability following a traumatic injury.
About open stabilisation
In Some circumstances, if there is further muscle or bone damage to your shoulder, these may need to be repaired in open surgery. Mr. Cole will speak to you as to which type of surgery will be most appropriate to your type of instability.
This is done with a small incision at the front of the shoulder. This is usually done to tighten up the capsule.
Preparing for your operation
This stabilisation surgery can be done as day surgery. This means that you won't normally have to stay overnight in hospital. However, you may feel more comfortable if you bring your own dressing gown, slippers and toiletries.
You will be having a general anaesthetic. This can make you feel woozy for a little time after the operation, so you will need to arrange for someone to take you home. It is important that you don't eat or drink anything for six hours prior to your admission into hospital, although you may drink water up to two hours prior to admission.
If you normally wear make-up or nail varnish, please remove it prior to your admission. You will also need to bring all prescribed medicines and supplements, in their original containers, with you to the hospital.
Understanding your operation
After admission, you will be seen by Mr. Cole and by your specialist anaesthetist. They will talk about the operation and the anaesthetic with you and, where possible, discuss your preferences. Nothing will be done without your permission on the day.
Anaesthetic and pain relief
The operation is carried out under a general anaesthetic. After your admission, you will be given a pre-med. This is usually in tablet or liquid form. This will help you relax before your operation
You will then be taken to the anaesthetic room, where you will be given the anaesthetic. This may either be a gas to breathe or an injection. This will be all you remember about the operation, as you will fall asleep at this point and awake after the operation in the recovery room.
Normally you will be given an interscalene nerve block during the operation. This acts as an excellent pain relief and for a short while after your operation your shoulder and arm may feel numb. When this wears off, your shoulder can feel more sore. You will be given some painkillers to take after the operation. When you begin to feel sensation returning to your shoulder (often a "pins and needles" feeling), you should start taking the pain medication that you have been given. Don't wait for your shoulder to start hurting, as pain is best managed before it gets acute. To keep the pain under control, use your medication regularly to begin with. After a couple of days, you can begin to lower the amount you take and then cease the medication altogether once any pain has subsided. If the pain does not seem to get better, or if you need more pain medication, please contact Mr. Cole.
A cold compress can also help with pain relief and swelling at the site of your operation. If you use an ice pack it is important you keep the wounds dry.
Risks
All operations involve a small element of risk. In stabilisation procedures these can include:
Complications relating to the anaesthetic such as sickness, nausea or rarely cardiac, respiratory or neurological issues (less than 1% each, i.e. less than one person out of one hundred).
Infection. These are usually superficial wound problems. Very rarely deep infection may occur many months after the operation (less than 1%).
Unwanted pain or stiffness in or around the shoulder (less than 1%)).
Damage to the nerves and blood vessels around the shoulder (less than 1%).
The need to re-do the surgery is rare. However the repair may fail and the shoulder become unstable again. This occurs in about 3-10% of cases.
Please discuss these issues with Mr. Cole if you would like further information.
Recovery
Follow-up appointments
You will usually be invited to attend an outpatient clinic about ten days to 2 weeks after your operation, where the wound will be examined and, if you have any, your stitches removed. After about six to eight weeks you will be asked to return so that Mr. Cole can check on your progress. You may discuss any concerns you have during these appointments. Alternatively, should you have a concern, you may telephone Mr. Cole's clinic at any time following your operation.
The wound
Arthroscopic stabilisation is a keyhole procedure. This means you will only have two to three small puncture wounds. You will not have any stitches, only small sticking plaster strips. With open surgery you will have a larger wound with stitches. Regardless of the type of wound you have, you will need to keep the area dry until they have healed, which is normally 10 to 14 days. You can wash or shower and use ice packs, but protect the wounds with a waterproof dressing. These will be given to you on your discharge from hospital Avoid using spray deodorant, talcum powder or perfumes near or on the scar. The dressing and stitches will normally be removed at your first follow-up appointment.
The sling
Your arm will be immobilized in a sling for about three weeks. It comes with a body strap which keeps your arm close to your body. This is to protect the surgery during the early phases of healing and to make your arm more comfortable.
You will be shown how to get your arm in and out of the sling. However, you should only take the sling off to wash or straighten your elbow. You may also remove it if you are sitting with your arm supported.
You may find your armpit becomes uncomfortable while you are wearing your sling for long periods of time. Try using a dry pad or cloth to absorb the moisture.
Sleeping
Sleeping may be uncomfortable for a while. It's best to avoid sleeping on the side of your operation. If you choose to lie on the other side, you can rest your arm on pillows placed in front of you. A pillow placed behind your back can help prevent you from rolling onto your operated shoulder during the night. If you are lying on your back to sleep you may find placing a thin pillow or small rolled towel under your upper arm or elbow will enhance your comfort.
Your recovery
Different people recover at different rates. However, you will need to keep your arm immobile within the sling for the first three weeks following your operation and will need to avoid certain movements for the six to eight weeks following that. For example, you should avoid moving your arm out to the side and twisting it backwards (in the way you would to put on a shirt or a seatbelt). The trick is to put your operated arm into the shirt first, so that it does not need reach up behind your back.
Your recovery can be divided into three phases:
Phase 1
This will last about three weeks. You will be wearing the sling and will need to keep your shoulder and arm still. This effectively means you will be one-handed, which will impact on your ability to do everyday activities.Phase 2
This will last eight to 12 weeks. After the third week of sling-wearing, you will be gradually weaned off its use and will start your physiotherapy. To begin with, you will only be able to complete activities at waist level and in front of your body. It may be six to eight weeks after your operation before you can use your arm above shoulder height.Phase 3
This phase can last six to eight months. At about eight weeks following your operation, you will be able to increase the level of your activities. You will be able to move your arm away from your body and may try slightly heavier tasks. You may start more vigorous activities, but will not be able to take part in contact sports for at least six months. You should regain strength and movement in your shoulder within six to eight months.
Complete recovery
Research has shown that after two to five years, about 90% of people have a stable shoulder with few limitations. Vigorous sports or those requiring repetitive overhead or throwing movements may require some adaptation for some people. However many people are able to return to previous levels of activity.
Driving
You may begin driving four to six weeks after your operation or when you feel comfortable. Check you can manage all the controls and it is advisable to start with short journeys. The seat belt may be uncomfortable to begin with, but your shoulder will not be harmed by it.
In addition, it is a good idea to check your insurance policy. Many insurers will require you to inform them of your operation.
Returning to work
The best time for you to return to work depends on which arm has been operated on, if you need to drive and on the type of work you do. If your job is largely sedentary and uses your non-operated arm, or requires minimal arm movements close to your body, you may be able to return to work between two and eight weeks after your operation. However, if you have a heavy lifting job or one with sustained overhead arm movements you won't be able to work for eight to twelve weeks. It is best to discuss this with Mr. Cole and with your physiotherapy team.
Returning to sport and leisure activities
Your ability to start these activities will be dependent on pain, range of movement and strength that you have in your shoulder. It is best to start with short sessions involving little effort and then gradually increase the effort or time for the activity. Your physiotherapy team will be able to give advice tailored to you and your situation. As general guidance, however, you can expect to have to wait this long for these sports:
- Cycling: 4-6 weeks
- Gentle swimming: 8-12 weeks
- Light sports or racquet sports using the non-operated arm: 10 weeks
- Racquet sports using the operated arm: 16 weeks
- Contact sports: 6 months
Physiotherapy
You will be shown exercises by the physiotherapist and you will need to continue with the exercises once you go home. They aim to stop your shoulder getting stiff and to strengthen the muscles around your shoulder. We have outlined these early exercises here. Your physiotherapy team will also devise a longer term programme tailored for you and your situation.
Use pain-killers, ice packs or both to reduce any pain before you begin exercise, if necessary. It is better to do short frequent sessions of physiotherapy several times a day, rather than one long session. Aim to exercise for five to ten minutes, four times a day.
It is normal for you to feel aching, discomfort or stretching sensations when doing these exercises. However, intense or lasting pain (such as pain that lasts for more than 30 minutes) is an indication to change the exercise by doing it less forcefully or less often.
Post operative exercises
Phase 1 Exercises
You can begin these exercises immediately after your operation.
1. Neck exercise (shown for right shoulder)
Do this exercise either sitting or standing
Turn your head and look to the left. Return your head to the centre, facing forward. Repeat 5 times
Turn your head to the other side and look to the right. Return your head to the centre, facing forward. Repeat 5 times
Tilt your head gently and slowly towards one shoulder. Return your head to the centre position. Repeat 5 times
Tilt your head gently and slowly towards the other shoulder. Return your head
to the centre position. Repeat 5 times
2. Elbow exercise (shown for left arm)
Do this exercise either standing or lying on your back
Straighten your arm and then bend it at your elbow
Repeat 5 times
Phase 2 Exercises
Begin these exercises a minimum of three weeks after your operation, as advised by Mr. Cole or your physiotherapy team.
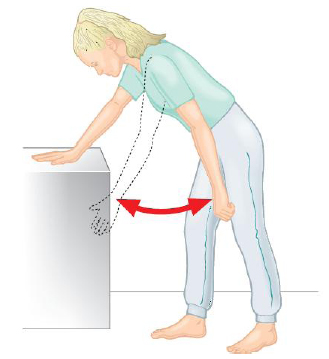
1. Pendulum (shown for left shoulder)
Lean forwards with support
Let your arm hang down
Swing your arm forwards and back
Repeat 5–10 times each movement
2. Arm overhead (flexion in lying) (shown for left shoulder)
Lie on your back on your bed or the floor
Support the arm of your operated shoulder with your other hand at the wrist and lift it up overhead
Do not let your back arch
Try to get your arm back towards the pillow or floor
You can start with elbows bent
Repeat 5–10 times
3. Arms behind back (shown for right shoulder)
Stand with your arms behind your back
Grasp the wrist of your operated arm
Gently stretch your hand towards the buttock of your un-operated side
Slide your hands up your back
Repeat 5 times
4. Hands clasped (shown for right shoulder)
Stand with your elbow bent and your arm close to your side (this can be done against a wall or door frame)
Clasp your hands together and push the palm of your hand into your other hand, taking care not to let it move
Hold for 10 seconds
Repeat 10 times
Build up to 30 repetitions
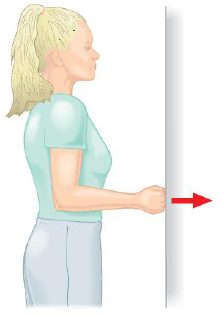
5. Wall hand push (shown for right shoulder)
Stand with your operated arm against a wall
Bend your elbow
Push the back of your hand into the wall, but do not let your arm move
Hold for 10 seconds
Repeat 10 times
Build up to 30 repetition
6. Back-to-wall elbow push (shown for right shoulder)
Stand with your back against the wall
Keep your operated arm close to your side with your elbow bent
Push your elbow back into the wall, but do not let your arm move
Hold for 10 seconds
Repeat 10 times
Build up to 30 repetitions
7. Side-to-wall elbow push (shown for right shoulder)
Stand sideways to a wall with your operated arm leaning against the wall
Keep your operated arm close to your side with your elbow bent
Push your elbow against the wall, but do not let your arm move
Hold for 10 seconds
Repeat 10 times
Build up to 30 repetitions
8. Face-to-wall fist push (shown for right shoulder)
Stand facing a wall, about 10cm away from the wall, so that your fist is
touching the wall without you needing to move your armKeep your operated arm close to your side with your elbow bent
Push your fist into the wall, but do not let your arm move
Hold for 10 seconds
Repeat 10 times
Build up to 30 repetitions
9. All fours movement (shown for right shoulder)
Kneel on all fours
Gently rock forwards taking the weight of your body through your arms
Keep your shoulder blade flat
Progress to lifting your unaffected arm up in the air (in different directions)
Repeat 10 -15 times
10. Wall, knee and full press-ups
Stand about 50cm - 100cm away from a wall with your palms flat on the wall at about shoulder height
Keep your back straight and your elbows under your body
Slowly bend your elbows so that you lean towards the wall in a press-up movement
Repeat 10-20 times
Progress to doing press-ups on all fours. Remember to keep your back straight and your elbows under your body
Repeat 10 to 20 times
When stronger, on the advice of your physiotherapist, you may progress to doing full press-ups
Phase 3 Exercises
Begin these exercises a minimum of eight to 12 weeks after your operation. A special programme will be devised for you by your physiotherapy team in consultation with Mr. Cole. They will concentrate on increasing the strength and mobility of your shoulder.
I would like to thank Professor Carr and Jane Moser of the Oxford Shoulder and Elbow Clinic for allowing us to reproduce some of this text and illustrations from their patient information